Background
Acute painful vasoocclusive episodes (VOEs) are the most common reason for hospitalization for adults with sickle cell disease (SCD) and significant predictors of mortality. The facilitators and barriers to providing quality care for adults with SCD in the inpatient setting are largely unknown. We aimed to explore inpatient SCD delivery models in the US, including access (or lack thereof) to quality care and sickle cell disease expertise.
Methods
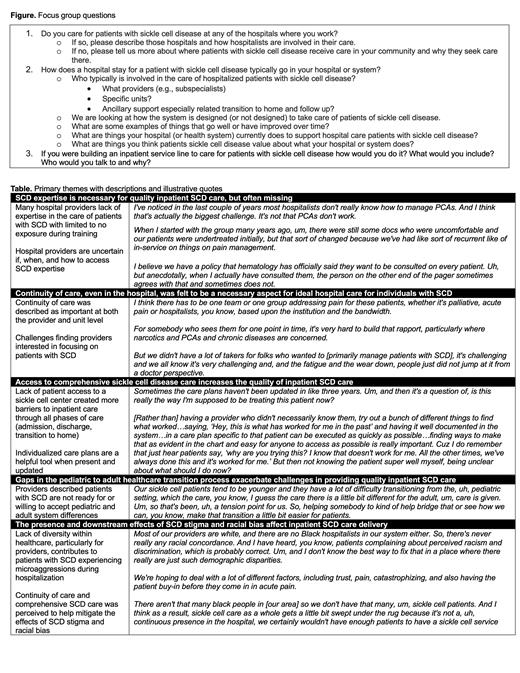
We conducted a multi-site rapid qualitative research study in order to evaluate a construct informed by literature review and clinical experience: variability between hospitals in the characteristics on models of inpatient SCD care delivery. We used virtual focus groups of practicing hospitalists in partnership with the Hospital Medicine Reengineering Network from across the United States. We developed an interview guide with open-ended questions and prompts through an iterative process to explore how inpatient SCD care is currently delivered in US hospitals with a focus on how these models of care delivery affect hospitalist practice (Figure). The open-ended questions explored topics ranging from hospitalists' training and experienceto the design of the health care system. Trained facilitators conducted four semi-structured focus groups with 11 hospitalists and one patient and family advisory council member. The facilitators took observation notes. Moderators summarized their group's overall findings for report to the larger group, serving as an opportunity for member checking and pattern identification. The focus groups lasted 35 minutes and report-out summaries lasted an additional 15 minutes. Recordings were de-identified and transcribed. We used rapid qualitative methods to explore perspectives of hospital-based healthcare providers including: having facilitators with expertise in the content area, collecting and analyzing data via multiple team members, and using templated summaries for each focus group question. Group summaries and transcripts were analyzed with thematic coding by two independent coders with feedback from the focus group moderators.
Results
Participants were from 12 adult university-based or university-affiliated hospitals. All hospitalists had experience taking care of hospitalized patients with SCD during their career, but many described how a change in practice location resulted in only seeing 1-2 patients with SCD per year. Hospitalists described a range of inpatient SCD care models from no specific model to a specific cohorted unit with associated providers. Participants unanimously expressed having provider and unit continuity of SCD care, and having accessible SCD expertise, as an ideal state. Individualized care plans were cited as a helpful tool for inpatient SCD care, but there were considerable challenges to their routine use. Primary themes are presented in the Table with explanations and correlative illustrative quotes.
Discussion and Future Directions
Hospitalists described wide variation in inpatient SCD care models. More inpatient SCD care support and infrastructure like individualized care plans were more commonly referenced by those hospitalists whose patients had access to a sickle cell center or SCD expert. We are using these data to inform a national survey to further describe and understand inpatient SCD care, if and how care plans are used, and determine next steps for improving inpatient SCD care quality.
Disclosures
No relevant conflicts of interest to declare.